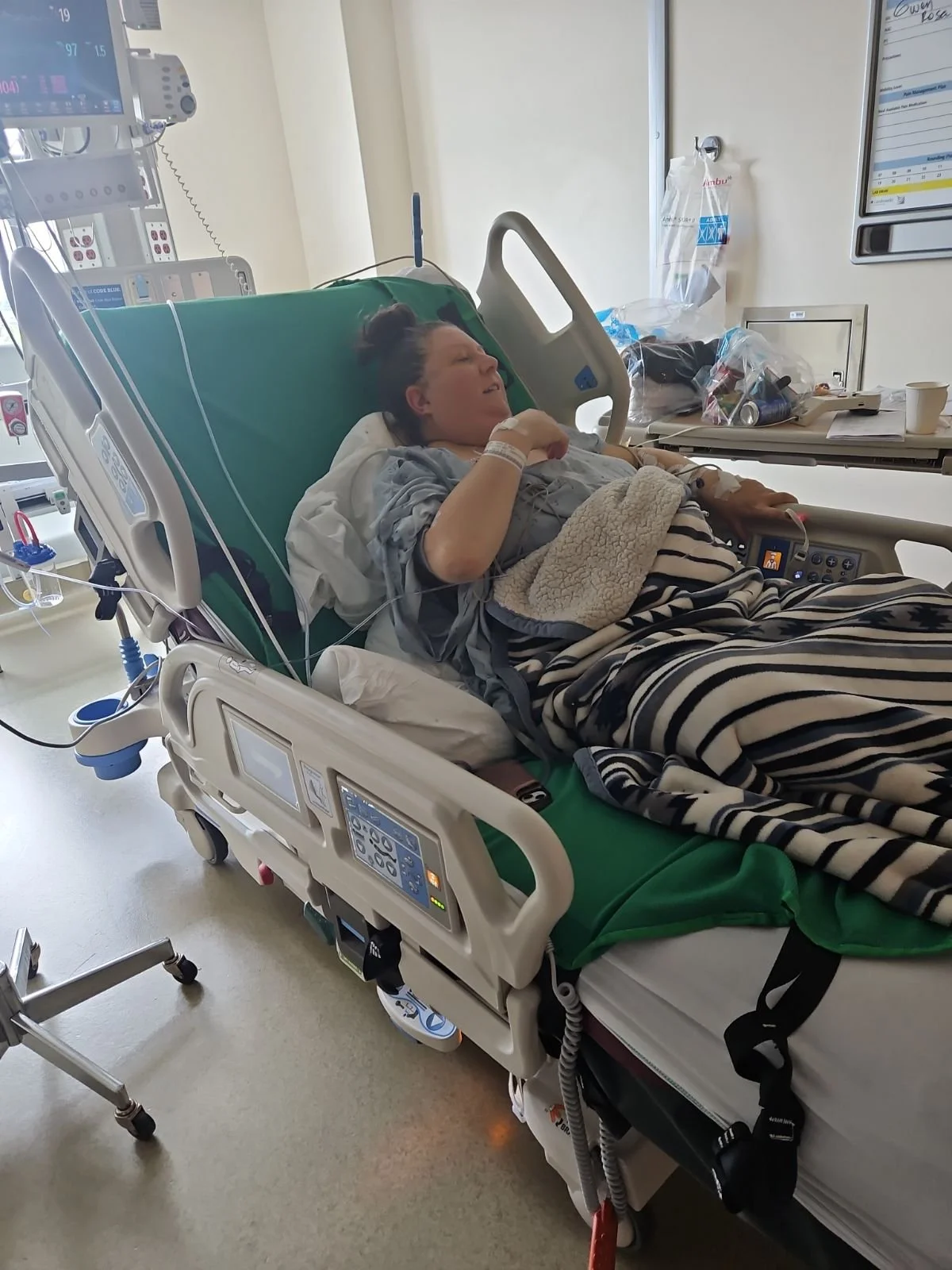
July 31, 2024 - Information Overload
My mom was finally in Seattle so today became information overload! We sat through a presentation all about Organ Transplantation, met with several members of the transplant team (Case Management, Nephrology, Nutrition, Social Work), underwent a Psychosocial Assessment and the remainder of the Stress Test.
Up to this point, I knew I was in Seattle being evaluated for a possible liver transplant, but I didn’t really know what all that entailed. The presentation was designed to provide us all that information as well as talk about the risk factors and success rates both on a national level and at Swedish Medical Center. The transplant team (spread across Seattle and Spokane) consisted of 5 RN Transplant Coordinators, 3 Transplant Surgeons, 4 Hepatologists, Social Work, Financial Coordinator, Dietician and Schedulers. I would have my initial consultation with most of them today.
Swedish Liver Transplant Program was established in 2009 with more than 385 transplants performed. They have an experienced Transplant Team focused on personalized and specialized care and partner with UNOS (United Network for Organ Sharing) for management of the SRTR (Scientific Registry of Transplant Recipients) database and LifeCenter Northwest (LCNW) that is responsible for organ procurement. Their success rate is as follows:
The quality of life after transplant was reported to be generally good with the longest survivor living over 40 years after transplant. There are a lot of factors that determine long-term survival but timely and consistent follow-up with your transplant team is essential.
Not everyone that needs a liver transplant can have a liver transplant. Those that may be good candidates for liver transplant include people with Acute Liver Failure, Advanced Chronic Liver Disease (viral, autoimmune or alcoholic cirrhosis, Non-Alcoholic Fatty Liver Disease, Hepatic Fibrosis, etc.), Metabolic Liver Disease and Unresectable Liver Cancer. However, there are several contraindications in which a candidate would be no longer eligible including Medical (uncontrolled infection/sepsis, bile duct or invasive liver cancer), Surgical (advanced heart or lung disease, extensive portal vein thrombosis) and Psychosocial (severe neurologic or psychiatric disease, lack of caregiving, lodging, financial factors, active alcohol/drug use). Additionally, liver transplant patients must completely abstain from alcohol, illicit drugs, non-prescribed medications and refrain/reduce the use of tobacco and marijuana.
Transplant Evaluation occurs in two phases with the first phase including:
Confirm diagnosis
Discover and correct preoperative problems – Is there anything so severely affecting survival that transplantation is inappropriate?
Discover and correct contraindications – Can the patient survive the operation and postoperative period?
Individual evaluations from:
Nurse Coordinator
Hepatologist
Transplant Surgeon
Social Worker
Dietician
Financial Counselor
Can the patient comply with the complex medical regimen required after transplantation?
As of today, my diagnosis had been confirmed (although the exact root cause was still in question) and they had begun working through phase 1 of the evaluation.
First up, I underwent a Nutrition assessment due to my inadequate energy intake related to End-Stage Liver Disease evidenced by poor appetite and nursing evaluation. I was currently on a low sodium diet with fluid restrictions and being given Ensure Max 3 times a day to have meals with. I couldn’t eat and really hadn’t been eating for weeks, so having to try and maintain at least 3 meals a day with Ensure Max was a lot for me and it was making me incredibly sick. I was agitated and really didn’t want to be talking about my nutrition now when all I could think about was staying alive. It was reported that when I was asked about my home diet, I was evasive and didn’t want to answer any questions, that I was very irritated, rolled my eyes, sighed and generally refused to participate in the visit. I was counseled on the importance of high protein diet and the accelerated starvation due to altered metabolism associated with end stage liver disease. If I continued to struggle with meeting the nutrition goals, I would be considered for a feeding tube particularly post-transplant.
I then underwent a psychosocial (severe neurologic or psychiatric disease, lack of caregiving, lodging, financial factors, active alcohol/drug use) assessment in which I was evaluated to determine if I was able to abide by the following:
Relocate with my caregiver to within a 1-hour drive of the hospital for a minimum of 6-8 weeks from the date of discharge after transplantation.
Acquire financial assistance for lodging and/or secure lodging at my own cost.
Secure at least two caregivers that will provide 24/7 care, medication management, assistance with daily activities and transportation to and from the clinic.
Complete DPOA (Durable Power of Attorney) paperwork in line with WA state LNOK (Legal Next of Kin) hierarchy.
Long-term abstinence from alcohol.
I met with case management in which it was determined that there were no barriers to me having and maintaining secure housing, utilities, transportation and no present food insecurities. My aunt Sheila was cleared as a secondary caregiver for Orthotopic Liver Transplantation from a psychosocial perspective. No care coordination or discharge planning needs were identified but Case Management would remain available should anything arise.
I then met with social work. This evaluation was probably the hardest so far. Not because it was physically demanding but it took a toll on me mentally and emotionally. They asked what seemed like a million questions, dug deep into very personal information and began the never-ending evaluation of my alcohol use patterns. Up to this point, they knew my diagnosis, but they still didn’t know the root cause. They had speculations of their own and often ignored the obvious explanations that led me to the ER in the first place 5 days ago. But they continued to try and find fault in my alcohol use patterns. Similarly to my admission day, I went through my consumption patterns, how much I drank, how long I’ve been consuming alcohol, times that may have led to heavier drinking and the reasoning behind it, family history of alcohol abuse, no cravings/withdrawals, no DUIs nor attending treatment and no reports of alcohol affecting every day life and/or job status. All indications show that I do not have a problem with alcohol abuse and therefore shouldn’t be considered as the sole cause of my end-stage liver disease.
Through their evaluation, it was determined that I had a history of using alcohol, tobacco and marijuana but have remained abstinent from alcohol for a couple weeks, tobacco for a few months (since February) and marijuana for 10-15 years but were recommending that I receive random tox screens and routine PEth testing to ensure that I remain adherent to lifelong abstinence moving forward and I was required to participate in outpatient treatment program required for liver transplant. This was insane to me!! Alcohol use and alcohol abuse were two entirely different things, and I did not abuse alcohol, yes I probably drank more than I should have, but I didn’t have an alcohol problem. There was no medical test showing that I had an alcohol problem, and my alcohol test was negative at time of admission, but they were simply making these determinations based on my verbal admission to my usage patterns. Again, ignoring the reason I am in the hospital in the first place but rather trying to put the blame elsewhere.
I was beyond frustration and finished talking to people at this point. The remainder of the evaluation concluded that I had a history of maladaptive coping mechanisms exacerbated by my illness and was recommended that I establish treatment with a licensed mental health professional but closely monitor my mood for exacerbation. Nothing like being kicked when you are down. All of this was absurd!!
Additionally, they determined that I was experiencing financial strain due to just beginning a new job 4 days before arriving to the ER and my insurance benefits were not available until September 1st. Fortunately for me, I had signed up for state insurance while I was temporarily unemployed due to my on-going health issues, so I automatically qualified for financial assistance. This didn’t dismiss the fact that transplant costs are significantly high, even with good health insurance and it is critical for long-term success to maintain consistent medical evaluation and on-going medication needs.
Finally, the day was coming to an end, and I would hopefully be able to relax. I still had to complete the second portion of my Stress Test but that will be easy compared to how emotionally draining the remainder of the day was. I was overwhelmed and filled with anxiety, so the plan is to temporarily treat my anxiety with Ativan and continue with Phase 2 of Transplant Evaluation tomorrow.